Researchers at the University College London, Institute of Ophthalmology, and Moorfields Eye Hospital, NHS Foundation Trust, UK, reported a study indicating that large disparities of genetic testing and results are required in the “diagnostic pathway” for inherited retinal diseases (IRD). While there has been significant improvements on genomic testing in recent years, the authors have stated that “around 40% (of patients) do not receive a definite genetic diagnosis after extensive genetic testing”. The recent paper, published in the journal British of Journal Ophthalmology, suggests that artificial intelligence (AI) may bridge current gaps in the “IRD care pathway” and that patients support a favourable attitude towards incorporating AI into diagnostic testing. The survey is the first to evaluate patient perspectives and considerations regarding the application of AI in the diagnosis of IRDs, significantly supportive of AI initiatives.
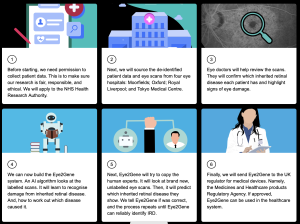
According to researchers, the average time to diagnosis for an IRD patient in Europe or America is presently 6.4(±9.1) years. Getting a definitive diagnosis for patients for a recommended 1 year timeframe is challenging due to extreme genetic heterogeneity, phenotypic variability and availability of clinical expertise for IRD many jurisdictions. In addition, interpreting novel or rare genetic variants can yield an inconclusive result, including “variants of uncertain significance”. Artificial intelligence (AI) can analyse large volumes of imaging data acquired from patients with IRDs, enabling identification of distinct patterns of genotype-phenotype correlations. The availability of connected data, formats and jurisdictions now have an opportunity to accelerate a diagnostic process and one example of such AI provides a “tool that is in development to aid genetic diagnosis is Eye2Gene”, an initiative supported by the National Institute for Health Research (NIHR) Biomedical Research Centre (BRC) at Moorfields Eye Hospital NHS Foundation Trust and UCL Institute of Ophthalmology, and also funded by a Moorfields Eye Charity Career Development Award. The Eye2Gene work located on https://eye2gene.com/#eye2gene and their summary approach outlines on the patient journey:
Researchers that conducted the survey used an online secure platform through registered charities in the UK, which provided support to patients with IRDs: Retina UK, Moorfields Eye Charity and Stargardt Connected. The survey was answered by 242 respondents, 80.2% of which were patients and the remainder were relatives, friends or caregivers. Following analysis of the data, the researchers confirmed that there was substantial variability in patient diagnostic journeys. The median (IQR) age of the participants was 53 (36–64) years and 57.4% were women, with the most common conditions were Stargardt disease (44.2%) and retinitis pigmentosa (RP) (43.0%). In terms of waiting times to see a specialist, the IQR was 1–4 years, the commute required IQR was 10–74 miles and number of visits to reach a diagnosis IQR was 2–4 (visits).
The results indicated that a substantial proportion of patients (35.8%) had a change in diagnosis in the patient journey and “the majority of respondents (>90%) were overwhelmingly in favour of the integration of AI into the IRD pathway to accelerate genetic diagnosis and improve care.” The researchers concluded that the IRD care pathway may potentially bridge gaps of knowledge using AI and the survey provides a favourable attitude towards incorporating AI into diagnostic testing of IRDs. According to the researchers, “the majority of the patients, as well as their companions, have a positive attitude towards AI being incorporated to improve their clinical care in the UK. These findings, which reflect the perspectives of patients, are valuable for informing and shaping policy on the integration of AI into the IRD care pathway.”