A systematic review and meta-analysis, performed by researchers at the School of Medicine, College of Medicine, Taipei Medical University, have shown a strong association between retinal vein occlusion (RVO) with an elevated risk of myocardial infarction (MI). Their research indicates that improved cardiovascular monitoring for RVO patients is essential to mitigate such MI risk, “underscoring the importance of proactive clinical care and further studies in this area”. The systematic review showed a relationship that could lead to improved preventive measures and management protocols for RVO patients, “thereby addressing a critical gap in the current literature and providing a basis for future research and clinical guidelines.”
Researchers have underscored that RVO and myocardial infarction significantly affect patient health and mortality. Both events, RVO and MI, cause a blockage or obstruction of blood flow and both conditions share common risk factors such as hypertension, diabetes and atherosclerosis, and are major contributors to cardiovascular-related events. The researchers in Taiwan conducted their study to investigate the possible association between RVO and MI, especially among younger individuals and consider how this relationship could lead to impact health for RVO patients. They conducted an exhaustive investigation of multiple databases using a PROSPERO protocol (University of York). The researchers identified 1,297 records and, following screening and assessment, twelve (12) studies were included for a systematic review and meta-analysis. Of the 12 studies, the number of patients ranged from 45 participants to 45,304 participants, most had a mean age of 60 years old, and having a prevalence of comorbidities of diabetes, hypertension and hyperlipidemia. The studies were diverse from countries, including Taiwan, the USA, Italy, Denmark, Korea and Japan, and this reflects a wide geographic distribution providing a generalizable outcome.
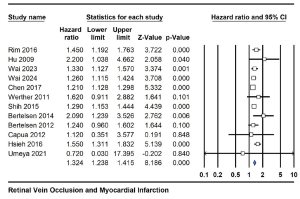
The results across the 12 studies showed that the relationship between RVO and the risk of MI had a pooled hazard ratio was 1.324 (95% CI 1.238, 1.415), presenting a statistically significant positive association, with a p-value was 0.0001. On a sub-group analysis, central retinal vein occlusion (CRVO) revealed a statistically significant hazard ratio of 1.691 (95% CI 1.142, 2.502), with a low p-value of 0.009. Forest plots show a graphical outcome of the association between RVO / CRVO and MI.
Figure 1. Forest plot depicting the pooled hazard ratio for the association between RVO and MI risk across twelve cohort studies. [Open access article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format when provided to the appropriate credit of: Chen et al. International Journal of Retina and Vitreous (2024) 10:86; https://doi.org/10.1186/s40942-024-00606-9].
Figure 2. Subgroup analysis of CRVO showing the hazard ratio and confidence intervals for the association with MI risk. [Open access article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format when provided to the appropriate credit of: Chen et al. International Journal of Retina and Vitreous (2024) 10:86; https://doi.org/10.1186/s40942-024-00606-9].
Commenting on the work, the researchers stated that, “these studies have emphasized that RVO often serves as an early warning sign for underlying systemic vascular diseases, which can manifest as stroke and other cardiovascular events. The identification of RVO as a predictor of stroke has led to recommendations for comprehensive systemic evaluation and prompt management of cardiovascular risk factors in patients presenting with RVO.” The meta-analysis reveals a strong association between CRVO and a 69.1% increased risk of MI, and RVO is linked to a 32.4% elevated risk of MI. In summary, “improved cardiovascular monitoring for RVO patients, particularly those with CRVO, is essential to mitigate MI risk, underscoring the importance of proactive clinical care.”