Researchers based at the Singapore National Eye Centre, and the Ophthalmology and Visual Sciences, Duke-NUS Graduate Medical School, Singapore, have published a report showing clear clinical distinctions between EYS- and USH2A gene variants associated with, relevant for diagnosis, counselling and natural history studies, and potentially define new outcomes for future clinical trials. EYS and USH2A are the most prevalent causes of RP in Asia, Japan and China. Their new study have shown overlapping clinical presentations capable to be distinguished “on a constellation of phenotypic features including disease onset and severity, refractive error, and fundus autofluorescence.” These diagnostic features may support a more effective diagnostic strategy for these common forms of RP.
Researchers have outlined that pathogenic variants in the EYS (eyes shut homolog) and USH2A (Usher syndrome type 2A) genes are responsible for a substantial proportion of retinitis pigmentosa (RP) worldwide and are the most prevalent genetic causes of RP in East Asia. Both genes are large – EYS is 9.4 kb and USH2A is 15.6 kb and both are essential for structural integrity and function of photoreceptors, associated with both syndromic RP (Usher syndrome) and non-syndromic autosomal recessive RP. These gene variants of RP cause generalized rod-cone degeneration albeit atypical forms have been reported with sectoral and irregular observations. The researchers commented that, “USH2A-associated RP has most commonly been reported as a typical generalized RP pattern of retinal involvement, whereas EYS-associated RP is associated with atypical retinal distributions that may be genotype-specific.” Up to now, there was “no established phenotypic features that can reliably discriminate between these two prevalent forms of RP beyond the presence of congenital hearing loss in USH2A-associated Usher syndrome.” Their current data collated valuable information which may likely motivate further research to support these RP patient cohorts.
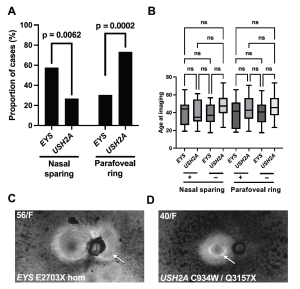
Following their analysis, 300 families with RP were enrolled with EYS- and USH2A-associated RP. USH2A cases were predominantly non-syndromic RP (75%) and EYS-associated RP was more severe in functional and structural outcomes, and patients were more myopic than USH2A (SE −3.31 vs. −0.69; P < 0.0001). EYS RP displayed peripapillary nasal sparing on autofluorescence imaging more frequently than USH2A (57.6% vs. 26.7%; P = 0.006), whereas USH2A cases more often had a parafoveal ring (73.3% vs. 30.3%; P = 0.0002). Multiple logistic regression identified diagnostic features with 83.2% accuracy in distinguishing between EYS and USH2A, validated in a second unrelated clinical cohort.
Figure 1: Autofluorescence imaging distinguishes between EYS and USH2A RP. (A) Peripapillary nasal sparing was more prevalent among individuals with EYS (P = 0.0019) whereas a parafoveal ring was more prevalent among individuals with USH2A (P = 0.0002). (B) Illustrative cases for both features are shown, along with the EYS and USH2A genotypes identified for each case. This is an open access article under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/), entitled: Phenotypic distinctions between EYS- and USH2A-associated retinitis pigmentosa in an Asian population. By Yeo EYH, et al., Transl Vis Sci Technol. 2025;14(2):16, https://doi.org/10.1167/tvst.14.2.16).
In conclusion, the authors of the paper stated that, “our findings have several important implications for clinical practice and research. The identification of phenotypic markers such as myopia and specific AF (autofluorescence) patterns provides valuable diagnostic tools for distinguishing between EYS- and USH2A-associated RP.” In addition, their analysis highlights areas for future research and therapeutic development, not least of all, gene editing technologies such as CRISPR/Cas9 which offer promising alternatives for correcting mutations in large genes of EYS and USH2A.