Researchers at the Institute for Molecular Medicine Finland (FIMM), University of Helsinki, and the Massachusetts Eye and Ear and Broad Institute of MIT and Harvard, Cambridge, have reported a new study showing a missense variant in the PTPRB gene is associated with central serous chorioretinopathy (CSC), varicose veins and glaucoma. The research, published in the journal Nature Communications, showed that the association of PTPRB with the pathologies had an odds ratio of 2.85, (P=4.5 × 10-9). PTPRB encodes vascular endothelial protein tyrosine phosphatase and the association was confirmed in a meta-analysis of 2,452 patients and 865,767 controls from 4 studies (odds ratio = 3.06, P = 7.4 × 10-15). According to the analysis of the data, the researchers commented that their findings “highlight the significance of vascular endothelial protein tyrosine phosphatase in diverse ocular and systemic veno-vascular diseases.”
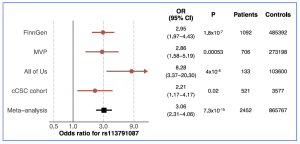
Figure 1. Associations of the PTPRB missense variant rs113791087 with central serous chorioretinopathy in 4 studies. The association of rs113791087 with central serous chorioretinopathy (CSC) was examined in 4 different studies. In all biobank-based studies (FinnGen, Million Veteran Program [MVP] and All of Us [see Methods in Nature Communications, 2025 16:4127)] included in the meta-analysis, patients with CSC were identified based on International Statistical Classification of Diseases codes, and all participants with age related macular degeneration were excluded from patients and controls following a harmonized study protocol. In the chronic CSC (cCSC) cohort, patients were identified from ophthalmological clinics based on expert review. Odds ratios (OR) and P-values were derived using logistic regression as implemented in Regenie (v2.2.4) in FinnGen, SAIGE (v1.3.0) in MVP, and Regenie (v3.2.2) in All Of Us. Association estimates and two-sided p-values were previously derived in the European cCSC cohort using the firth bias-corrected likelihood ratio test (see Rämö, JT et al Nat Comm, 2025) 16:4127). [This work is an open access content, licensed under the CC BY-NC-ND license (http://creativecommons.org/licenses/by-nc-nd/4.0/), authored by Rämö, JT et al., entitled, “Rare genetic variation in PTPRB is associated with central serous chorioretinopathy, varicose veins and glaucoma”, published in Nature Communications ( 2025) 16:4127, https://doi.org/10.1038/s41467-025-58686-6].
Central serous chorioretinopathy (CSC) is a maculopathy with a thickened and dilated choroidal vasculature, retinal pigment epithelium (RPE) detachments and subretinal fluid (SRF) and the disorder may manifest in individuals between 30-50 years of age with decreased visual acuity. The incidence can range between 5.8:100,000 and 34:100,000 in different populations. The researchers commented that vascular remodelling in CSC has been “compared most closely to varicose veins, although the changes are on a much smaller scale. Varicose veins are a common disease affecting approximately 20% of the population (females more than males) and represent a weakening of the vessel wall with resultant vascular dilation in the lower extremity (typically in the greater and lesser saphenous veins)”. In their current study, the researchers identified genotype data from 1,477 patients and 455,449 controls in the FinnGen dataset, showing the association with a missense variant (rs113791087) in PTPRB (odds ratio=2.85, P = 4.5 × 10-9) and was prioritized as “the likely causal variant by statistical fine-mapping” and “an increased risk of varicose veins and with a reduced risk of glaucoma”.
Following analysis, the researchers have proposed that ocular and systemic vascular diseases highlight a potential role for vascular dysfunction in central serous chorioretinopathy and this may provide an opportunity to identify novel therapeutic options. Commenting on their paper, the authors stated that a “genetic finding has illuminated the Tie-2 and VE-Cadherin pathways as important in CSC, an area of study that was not under investigation previously but that may be important for therapeutic advancement.” The same authors published a case series of patients with chronic CSC treated with intravitreal faricimab (an Ang-2 blocker and thus a Tie-2 activator). Fourteen of sixteen treated eyes (14/16) were found “to have reduced disease activity in response to the medication, providing additional evidence that this genetic finding is highly relevant” (see Am. J. Ophthalmol. 269, 246–254 [2024]).