Researchers at the Department of Ophthalmology, Boston Children’s Hospital, and the Harvard Medical School, have reported that the interface of photoreceptors and RPE in Stargardt disease (STGD1) patients have shown a “profile of the hyperreflective bands differed dramatically between patients with STGD1 and controls”. In their study with STGD1 patients, the outer nuclear layer (ONL) was thinner, and the distance from the external limiting membrane (ELM) to retinal pigment epithelium (RPE) was shorter, compared to controls. In addition, biomarkers of mitochondrial activity and respiratory efficiency was lower than in their age-matched controls. While certain cones and rods were present in their dataset, the researchers suggest that photoreceptors could be targeted for pharmaceutical treatment, thereby protect and mitigate vision loss in patients with STGD1.
STGD1 is an inherited disorder that can cause vision loss in children and young adults with an estimated 30,000 people affected in the U.S. and more than 150,000 worldwide. The disorder is caused by variants in the photoreceptor-specific ABCA4 gene, which encodes the adenosine triphosphate-binding cassette, subfamily A, member 4. The gene encodes a transporter protein within retinal photoreceptor cells facilitating the active transport of potentially toxic retinoid compounds removing toxic by-products from the visual cycle. A number of pathogenic variants within certain introns of the ABCA4 gene may result aberrant splicing of the gene – including pseudogenes – essentially non-functional segments of DNA. Loss of the protein results in the accelerated dimerization of vitamin A, forming toxic by-products that irreversibly damage the retina, resulting in progressive vision loss. In their cohort recruited to the study, the severity of the biallelic genotype ranged from effectively double null, to variants producing protein of less than half the normal functionality, to only mildly degraded protein functionality.
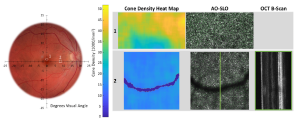
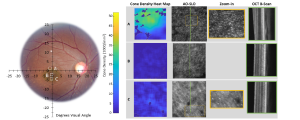
In their current research, adaptive optics (AO) imaging technologies enhance the resolution of the scanning light ophthalmoscopy (SLO) and optical coherence tomography (OCT) by correcting optical aberrations in the eye thereby allowing a cellular-level resolution and quantification of changes in cells non-invasively. This further interrogates the pathobiology of surviving STGD1 photoreceptors and the imaging data provide a significant insight with the living tissue.
In Figure A, a healthy control shows: Far-left fundus photograph of a healthy control (right eye); location and size of AO Scan 1 and Scan 2 are as indicated. Left column—cone density heat maps. Center column—AO-SLO cone images with identified cones (green dots). Right column—OCT B-scan at the location indicated by the green line on the AO-SLO. (Further detailed in the open access data available in De Bruyn et al, The Surviving, Not Thriving, Photoreceptors in Patients with ABCA4 Stargardt Disease, Diagnostics 2024, 14(14), 1545; this article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https:// creativecommons.org/licenses/by/ 4.0/).
In Figure B, a STGD1 patient shows, patient 4, right eye. Format is similar to that of Figure A, with the zoom-in (yellow square on the AO-SLO) column added. * (in the fundus image) in the superior retina, at ~10° is the patient’s preferred retinal locus for fixation (PRL). (Further detailed in the open access data available in De Bruyn et al, The Surviving, Not Thriving, Photoreceptors in Patients with ABCA4 Stargardt Disease, Diagnostics 2024, 14(14), 1545; this article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https:// creativecommons.org/licenses/by/ 4.0/).
In the Boston analysis, the researchers commented that, “this study of surviving, but not thriving”, showed clear dystrophy in the fine structure of the inner segment in STGD1 patients, despite the small sample of patients covering a range of ages and clinical presentations. In addition, the study and those of other researchers, indicate that surviving STGD1 photoreceptors are not rare and this may lead to suggestions for early pharmaceutical intervention. In conclusion, the researchers stated that, “through the study of the optical correlates of the metabolic machinery in these surviving photoreceptors, we are led to consider a pharmaceutical approach to protect these photoreceptors. A real-world challenge remains how to identify patients with STGD1 before any vision loss. With the development of genetic screening programs, there is hope that such can pertain to Stargardt disease”.